The history and development of penicillin as an antibiotic.
The Discovery of Penicillin
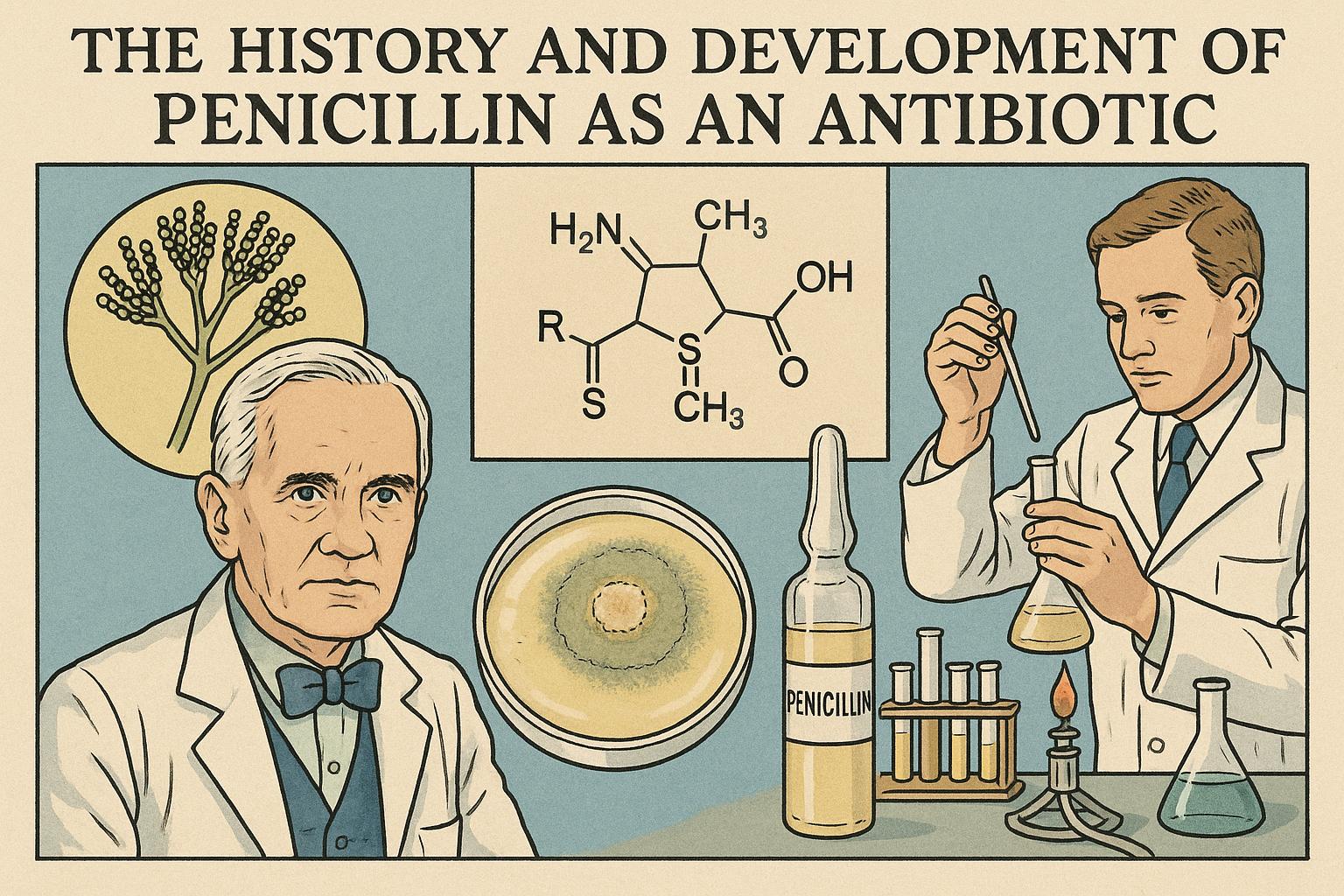
The discovery of penicillin stands as one of the pivotal moments in the history of medicine. Its story is not just about scientific curiosity but also about the interplay of chance and perseverance. The journey began in 1928, spearheaded by the Scottish bacteriologist Alexander Fleming. During his time at St. Mary’s Hospital in London, Fleming was engaged in studies of the Staphylococcus bacteria. It was during these studies that he made an observation that would eventually change the course of medical science. Fleming noticed that a mold had contaminated one of his Petri dishes. Upon closer inspection, he realized that this mold, later identified as Penicillium notatum, seemed to be inhibiting the growth of the bacteria around it.
Fleming’s curiosity led him to delve deeper into the properties of the mold. He recognized that the substance being produced by the mold had significant antibacterial properties. In 1929, Fleming published his findings. However, despite the importance of this discovery, Fleming himself did not fully grasp the potential of the substance he had unearthed. He lacked the necessary resources and expertise to extract and purify the substance, and as such, his work did not immediately lead to practical applications.
The Role of Howard Florey and Ernst Boris Chain
The real journey towards the development of penicillin as a practical antibiotic only gained momentum much later. In the late 1930s, two other scientists, Howard Florey and Ernst Boris Chain, both working at the University of Oxford, revisited Fleming’s neglected research. They saw the promise in Fleming’s observations and decided to overcome the challenges that had halted Fleming’s progress. By 1939, they embarked on a project to purify penicillin and evaluate its therapeutic potential.
These efforts bore fruit in 1940 when Florey and Chain were able to demonstrate penicillin’s efficacy in protecting mice from bacterial infections. This was a crucial milestone, as it provided concrete evidence of penicillin’s potential as a treatment for bacterial infections in humans. With these findings, the stage was set for the first human trials.
The First Clinical Trials
The success of the experiments on mice led the researchers to cautiously proceed to human trials. In 1941, penicillin was administered to a policeman who was battling a severe bacterial infection. The results were promising, as the patient’s condition initially improved. However, the limited supply of penicillin at the time meant that the treatment had to be halted prematurely due to exhaustion of the available penicillin, and the patient later succumbed to the infection.
This incident highlighted two crucial issues: the enormous potential of penicillin to change medical treatment and the dire need for large-scale production. The lack of sufficient quantities of penicillin was a glaring obstacle that had to be addressed for it to become a viable treatment option.
Mass Production and World War II
The onset of World War II added urgency to the production of penicillin. The Allied powers recognized its potential to not only revolutionize medical practice but also save countless wounded soldiers’ lives. In response, the United States and the United Kingdom launched collaborative efforts to scale up the production of penicillin. This collaboration led to significant advancements in production methods.
A turning point occurred at the Northern Regional Research Laboratory in Peoria, Illinois, where researchers developed deep-tank fermentation techniques. This innovation marked a departure from the slow and labor-intensive surface culture methods initially used. By 1943, thanks to these advancements in fermentation and production technology, penicillin was available in sufficient quantities to be deployed on the battlefield. It proved invaluable for treating infected wounds, transforming wartime medical care and significantly decreasing mortality rates from bacterial infections.
The Impact of Penicillin on Modern Medicine
The success of penicillin heralded a new era in medicine, often referred to as the beginning of the age of antibiotics. Penicillin not only treated infections effectively but also paved the way for the discovery and development of a range of other antibiotics. This pharmacological revolution had a profound impact on public health, leading to dramatic reductions in mortality rates from bacterial infections.
While penicillin remains a cornerstone in modern medicine, its widespread use has also introduced challenges. One of the most pressing issues today is the rise of antibiotic resistance. The misuse and overuse of antibiotics have led to the emergence of resistant strains of bacteria, diminishing the effectiveness of antibiotics like penicillin. This situation underscores the ongoing need for research in antimicrobial therapies and the continuous development of new drugs to stay ahead of resistance.
In conclusion, the discovery and development of penicillin stand as a testament to human ingenuity, curiosity, and the power of scientific collaboration. It highlights the potential of accidental discoveries to unravel groundbreaking advancements and reminds us of the constant evolution of challenges in medical science. The journey of penicillin, from a chance observation to a life-saving drug, remains a remarkable narrative of hope, persistence, and the relentless pursuit of knowledge.