How insulin regulates blood sugar in diabetes.
Understanding Insulin’s Role in Blood Sugar Regulation
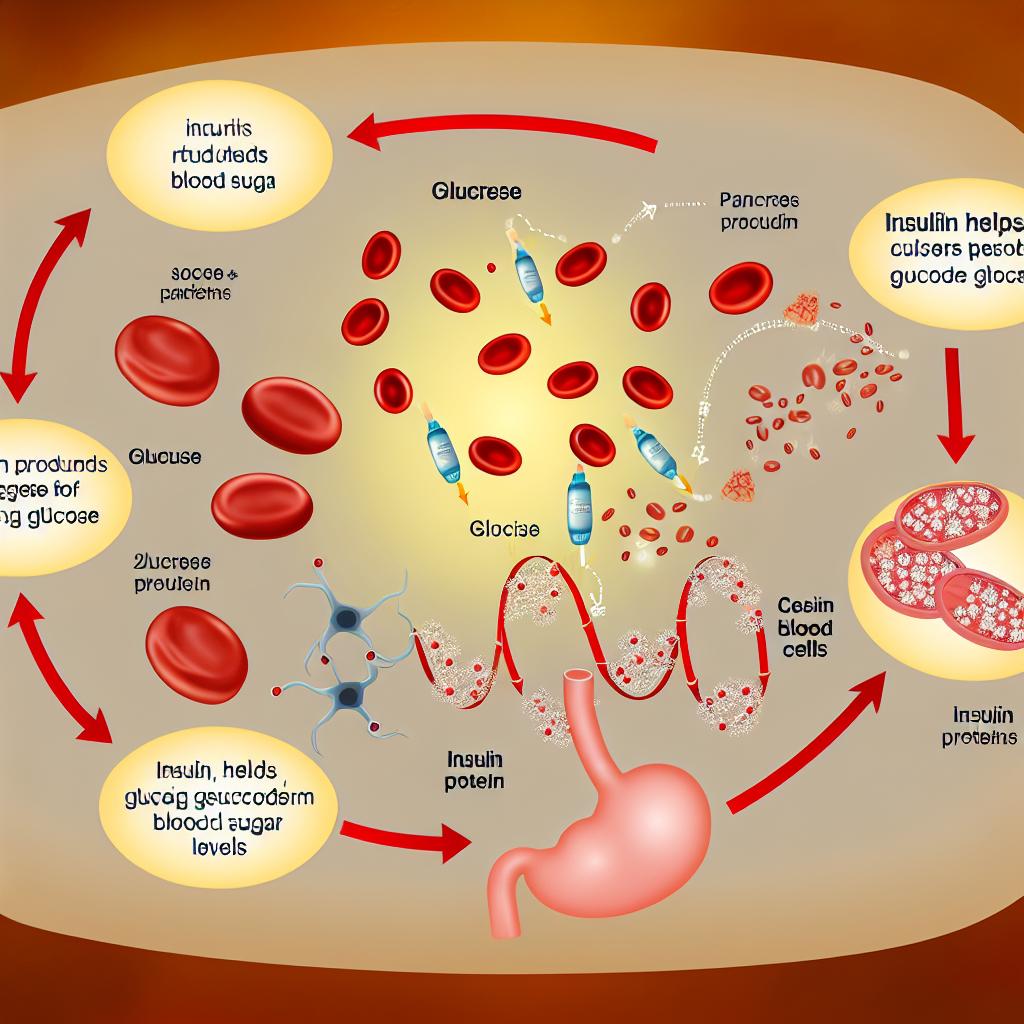
Insulin is a vital hormone produced by the pancreas, playing a significant role in regulating blood sugar levels. This regulation is crucial, especially for individuals with diabetes, where the body’s ability to produce or respond to insulin is impaired.
The Function of Insulin
When you consume carbohydrates, your body breaks them down into glucose, a simple sugar. This glucose enters the bloodstream, causing blood sugar levels to rise. Insulin is then released by the pancreas to help manage these rising sugar levels. Its primary function is to facilitate the uptake of glucose into cells, where it can be used for energy or stored for future use.
Mechanism of Action
Once insulin is released, it binds to insulin receptors on cell membranes, allowing glucose channels to open. This process ensures that cells can take in glucose effectively, thus lowering blood sugar levels to a normal range. Ensuring proper glucose uptake is essential for maintaining energy balance and overall health.
By binding to its receptors, insulin triggers a cascade of biochemical signals within the cell that encourage glucose uptake and utilization. Each cell is equipped with these receptors, providing a method for insulin to exert its effect universally throughout the body. Moreover, insulin facilitates glucose storage in the liver and muscle cells in the form of glycogen. This storage process is crucial as it helps maintain blood glucose levels during fasting or in between meals.
Insulin Resistance
In individuals with type 2 diabetes, the effectiveness of insulin is often compromised due to insulin resistance. This condition arises when cells fail to respond properly to insulin, necessitating higher insulin levels to maintain normal blood sugar. Over time, the pancreas may struggle to keep up with the demand, leading to elevated blood sugar levels.
Insulin resistance is associated with several risk factors, including obesity, physical inactivity, and genetic predisposition. The mechanism behind insulin resistance involves the reduced sensitivity of insulin receptors, which hampers the proper signaling required for glucose uptake. Consequently, this can lead to a condition known as hyperinsulinemia, where excessive insulin is present in the blood, eventually exhausting pancreatic function.
Insulin Management in Diabetes
For people with diabetes, managing insulin levels is critical. Those with type 1 diabetes require regular insulin injections because their bodies do not produce insulin. In contrast, individuals with type 2 diabetes might use a combination of lifestyle changes and medication to improve insulin sensitivity and control blood sugar levels.
Insulin Therapy
Insulin therapy is a common treatment for managing diabetes. This involves administering insulin injections to mimic the body’s natural insulin cycles. Proper dosage and timing are essential to avoid blood sugar spikes and drops.
For individuals with type 1 diabetes, insulin therapy is the cornerstone of disease management. Multiple daily injections or the use of insulin pumps help stabilize blood glucose levels. The insulin types used can vary from rapid-acting to long-acting, each playing a specific role in managing glucose appearance after meals or maintaining baseline levels during fasting.
In type 2 diabetes, cases that do not respond adequately to lifestyle modifications and oral medications may require insulin therapy. Some individuals might require a basal insulin dose to control blood sugars overnight and between meals, while others may use a combination of basal and bolus insulin.
Lifestyle and Diet
A balanced diet and regular exercise can significantly impact insulin sensitivity. Reducing simple carbohydrate intake and consuming more fiber-rich foods can help manage blood sugar levels effectively. Exercise enhances the body’s ability to use insulin, improving overall glucose uptake.
Maintaining a healthy weight is another critical aspect of improving insulin sensitivity. Weight loss, especially in overweight and obese individuals, has been shown to reduce insulin resistance. Additionally, maintaining a consistent meal schedule helps in stabilizing blood sugar levels, reducing the potential for drastic fluctuations.
Physical activities, including both aerobic and resistance training, promote insulin efficiency by increasing muscle glucose uptake and enhancing mitochondrial function within muscle cells. Regular physical activity can lead to long-lasting benefits in blood sugar management.
Conclusion
Understanding how insulin works and its role in blood sugar regulation is fundamental for individuals living with diabetes. By managing insulin levels through therapy and lifestyle modifications, it is possible to maintain blood sugar within a target range and reduce the risk of complications associated with diabetes.
The journey to managing diabetes effectively is a comprehensive endeavor, incorporating medical guidance, self-monitoring, and adopting healthy lifestyle practices. Educating oneself about insulin function and the body’s metabolic requirements greatly empowers individuals to take control of their condition. Ultimately, maintaining a fine balance in blood sugar levels is key to preserving health and preventing long-term complications associated with this chronic condition.
