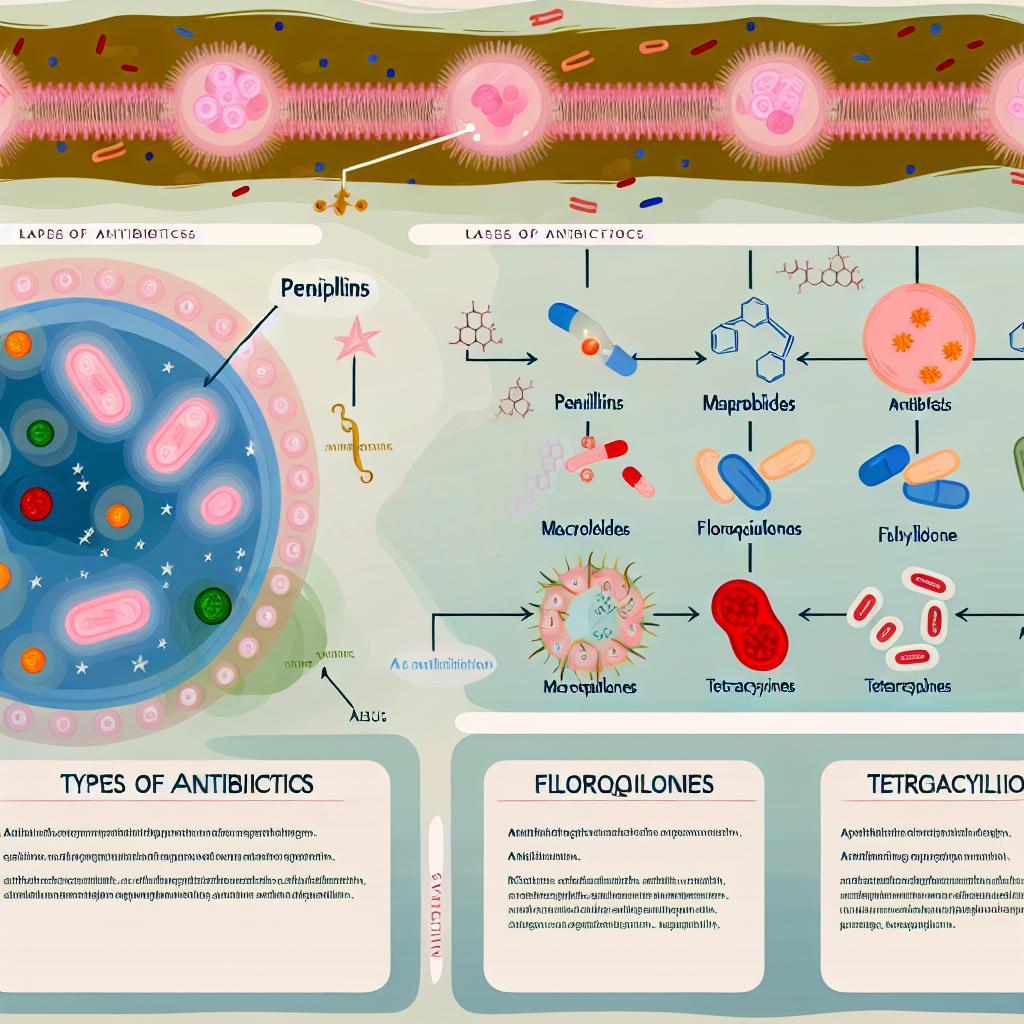
The different types of antibiotics and how they work.
Understanding Antibiotics
Antibiotics have evolved as indispensable tools in the realm of medicine, providing the means to effectively combat bacterial infections. These potent drugs work by either eradicating the bacteria or inhibiting their proliferation, thus playing a pivotal role in modern healthcare by treating diseases that were once potentially fatal. The diversity of bacterial infections necessitates the development of various antibiotics, each with unique mechanisms designed to address specific bacterial challenges.
Classification and Mechanisms of Antibiotics
The classification of antibiotics is primarily based on their chemical structure, spectrum of activity, and mechanism of action. Given the complexity of bacterial infections, it is essential to match each antibiotic to the specific bacteria it can effectively combat. Many antibiotics target bacterial cell walls, protein synthesis, or DNA replication, and their discovery and development have marked significant milestones in medical history.
Penicillins
Penicillins were among the first antibiotics to be discovered, revolutionizing the treatment of bacterial infections. They operate by targeting the bacterial cell wall, an essential structure for bacterial viability. Penicillins inhibit the synthesis of peptidoglycan, causing the bacterial walls to weaken and ultimately rupture. This renders them particularly potent against Gram-positive bacteria, which possess thick peptidoglycan layers. Despite their longstanding use, penicillins continue to be a cornerstone in antibiotic therapy due to their efficacy and safety profile.
Cephalosporins
Cephalosporins share a similar mechanism with penicillins, disrupting bacterial cell wall synthesis. However, they are classified into generations, each with an expanded spectrum of activity. This broadens their utility, allowing them to target a variety of infections ranging from uncomplicated skin infections to severe conditions like meningitis. The evolution of cephalosporins over generations has enhanced their ability to overcome bacterial resistance, making them a versatile option in antibiotic treatment.
Macrolides
Macrolides are a class of antibiotics that includes drugs such as erythromycin and azithromycin. They work by blocking protein synthesis within bacteria, disrupting ribosomal function crucial for bacterial growth and replication. Macrolides are often prescribed for respiratory tract infections and are a preferred alternative for patients allergic to penicillin. Their ability to concentrate in tissues and penetrate cells makes them particularly effective against intracellular pathogens.
Tetracyclines
Tetracyclines inhibit bacterial protein synthesis by preventing the addition of amino acids to peptide chains, effectively halting bacterial growth. This class of antibiotics has a broad spectrum of activity against a range of bacteria, making them useful for treating conditions like acne, Lyme disease, and various respiratory and urinary tract infections. Tetracyclines are known for their ability to penetrate and accumulate in tissues, providing therapeutic effects at the site of infection.
Quinolones
Quinolones, such as ciprofloxacin and levofloxacin, are synthetic antibiotics that target bacterial DNA synthesis. They achieve this by inhibiting the enzyme DNA gyrase, essential for the replication of bacterial DNA. Quinolones are considered broad-spectrum antibiotics and are often reserved for treating more severe infections. Their robust activity against a wide range of pathogens, coupled with their excellent tissue penetration, makes them valuable in cases where other antibiotics might fail.
Aminoglycosides
Aminoglycosides, including gentamicin and amikacin, function by binding to bacterial ribosomes, leading to the production of defective proteins. This disruption in protein synthesis invariably results in bacterial death. Clinically, aminoglycosides are primarily used against life-threatening infections caused by Gram-negative bacteria. Their potent antibacterial action is often enhanced through combination therapy with other antibiotics, providing a synergistic effect.
Sulfonamides
Sulfonamides exert their antibacterial effects by interfering with bacterial cell metabolism, specifically inhibiting the synthesis of folic acid, a vitamin-like compound vital for bacterial growth. They are often used in combination with other drugs to broaden their effectiveness against diverse bacterial species. Their historical significance and continued use illustrate the long-standing role of these antibiotics in medicine.
Bacterial Resistance and Considerations
A major challenge faced in the use of antibiotics is the emergence of bacterial resistance, exacerbated by the overuse and misuse of these drugs. Bacterial resistance threatens the efficacy of antibiotics and poses significant public health concerns. It is crucial for antibiotics to be prescribed judiciously and for patients to adhere to the complete course of treatment to mitigate the risk of resistance. Continued research and development in this field are essential to keep pace with evolving bacterial strains.
Future Directions and Innovations
The field of antibiotic research is ever-evolving, with advancements aimed at developing new classes of antibiotics and improving existing ones to combat resistant strains. By understanding the varied mechanisms and types of antibiotics, healthcare providers can better strategize their use in clinical practice. This ongoing innovation is crucial for maintaining the efficacy of antibiotics in fighting bacterial infections and addressing the challenges posed by resistant bacteria. Through continued dedication to research, the medical community strives to safeguard the health of populations worldwide.
In closing, antibiotics have dramatically transformed the landscape of bacterial infection treatment. Their diverse mechanisms and targeted action against bacteria render them an integral component of modern medicine. Ensuring their effective use requires not only medical expertise but also responsible stewardship, paving the way for future advancements and innovations in the battle against infection and resistance.
